The Back Story
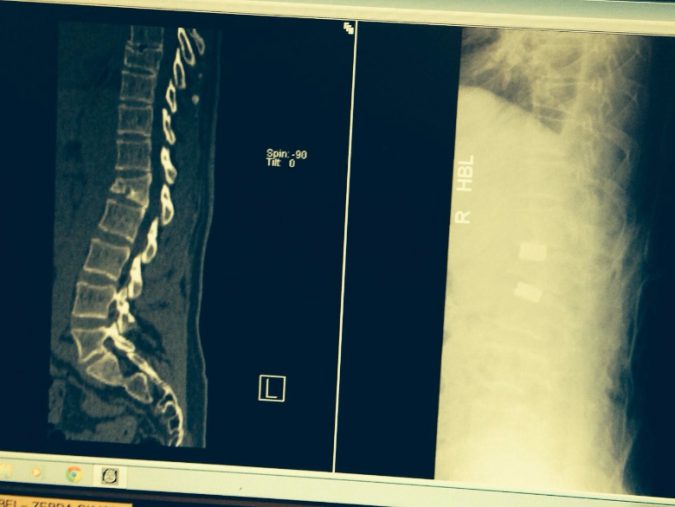
As the weeks tick by one by one, I inevitably have time to reflect on the journey that has brought me to this forced hiatus. I am guessing that over the last six years I have had about two hundred doctor’s appointments, a couple of hundred x-rays, about 30 MRI scans and a dozen or so Spec CT scans. As well as three surgeries and many hundreds of physio and osteo sessions. None of that list sounds ideal or an efficient use of anyone’s time and resources, so in retrospect the question that hovers around is - could I have managed the injury better? Who knows but I did my best and managing it all has sometimes felt like a full-time job. After the initial accident in October 2011, when I put a wedge fracture into my spine of just over 50%, the prognosis and therefore treatment plan seemed far from certain. I was passed around endlessly from expert to expert and nobody seemed to know what the best treatment plan was. The main problem being the chasm between a conservative treatment plan (phsyio/physical therapy) and invasive and inherently fraught corrective surgery. I remember very early after the accident that I was becoming aware of my spine bulging painfully at the L1 level and the pain continued to torque up like a ratchet.
Battle of The Bulge
This bulge (kyphosis) has been with me for six years, digging into the back of every chair, bath, bed or surface I that sit against or lie upon. It has been a defining feature of my body, dictating my alignment, function and balance since the accident. But now subsequent to surgery five weeks ago that bulge seems to have gone (there is still surgical swelling) and my spine seems to be correctly aligned for the first time in six years. This spinal correction is profound on both a physical and emotional level. And in the early weeks as I dutifully perform my 2 x 20 minute mobilisation programme that was prescribed by Mr Tucker, I have had to learn to propriocept the simple act of walking and balance again. My wife constantly reminds me not to hunch back into my old posture as we walk together; it is so strange to have to be reminded to walk like a normal biped. Maybe I never did.
Early Success?
In my first Journal on this latest round of surgery I defined what would constitute success at this point post procedure –
“This time my expectation is better measured. I want to get out: without any infection, without any nerve damage, my spine posture corrected, and with sound foundations for spine fusion. The rest can wait.”
Within these terms I think the early signs are that surgery has been a success. I was rightly measured in my expectation and I am still now restrained in any judgement of success - I don’t have any nerve damage I can feel, I don’t seem to have an infection and so far it seems my spinal profile has changed. But I am so gun-shy after the failure of the last surgery that I am ever vigilant in review and diligent in my rehab. My ongoing pain levels are inexorably linked to activity. It is a binary relationship. And the very worst thing I can do is sit down, which is something normal life requires regularly, from breakfast to answering an email and everything in between.
Surgical Top Trumps
Both Journals have generated interesting feedback from people who have had, or are about to have surgery, or they have a family member that is in the run up to spine surgery. I am more than happy to provide my perspective beyond the confines of these Journals, and completely understand the natural fear and trepidation that surrounds the words spine and surgery when they appear in the same sentence. Actually the concept of spine surgery bothered me less this time than last. Spine surgery is slightly bizarre because it overlaps two distinct branches of medicine – neuro-surgery and orthopaedic surgery. Last time I elected to have surgery with a respected neurologist spinal surgeon, probably because the word ‘neurologist’ sub-consciously ameliorated those worst fears of nerve damage. In a metaphorical game of Surgical Top Trumps a neurosurgeon must surely trump a spinal orthopaedic surgeon? The latter after all is merely a glorified carpenter with sharper saws and disinfected screws and bolts? Well so far that is not my experience. My kyphotic or Gibbus deformity was a mechanical deformity, therefore needed a purely mechanical fix. Morevover I completely engaged with the fact that Mr Tucker was obsessed with angles and mechanical integrity and structure. He had a plan to approach my spine from the front and back to remove the old vertebrae and all the redundant metal-work and replace it with a bigger cage and screws and rods up the back of my spine – it is called a 360 degree Lumbar Corpectomy. My friend and osteopath, Alex Fugallo, attended the entire surgery and reported back that the limited conversation between the team over the six or so hours, generally centred around Mr Tucker's over-riding goal of getting the thoracic/lumbar junction back to zero degrees. Thus far the Orthopaedic surgeon has succeeded where the neurosurgeon failed, in terms of the spinal re-alignment remit at least.
Encouraging Fusion
As one of my very eloquent and well informed clients (who is just recovering from his own surgery) pointed out to me in an email – the huge elephant in the room in my Journals is whether or not spinal fusion actually takes place in the coming months? In that context what can I do to try and encourage the fusion process?
Here is the list I have been given that could encourage bone-growth and therefor fusion -
1. don’t smoke
2. stay hydrated
3. keep walking (loaded bone is good bone remember)
4. stay positive and relaxed
5. be diligent with my physio and live and eat well.
Hence I am currently I am fully subscribed to all of the above.
Five Week Check
After five week of secluded isolation, it is a bit of a shock to be disgorged onto the pavement outside Marylebone Station, into the thrum of a London morning. How quickly we become our own jailers? It was very pleasant to see Mr Tucker again. The surgeon-patient relationship must be a difficult one. In their entire life the patient will probably never have cause to trust another individual so completely, that they are once virtually estranged from. The surgeon for their part has to strike an impossible balance of professional distance with personal empathy and engagement. Mr Tucker does a pretty good job, erring on the concise side, but I have always intrinsically trusted him. The consultation goes well within its terms. It has been five weeks since I was anything other than bolt upright or lying down, so when Mr Tucker instructs me to reach for my toes I start shaking long before I get near the general post-code of my knees. But he seems moderately happy with that and visibly delighted by my general posture and alignment. A few more perfunctory stretches and bends and I am back on the street emboldened with my new instructions:
1. No more embolism socks (pictured)
2. No more brace when mobilising (pictured)
3. Time to start physio in earnest (Shaun ex-Cyclefit to supervise)
4. I can have a very occasional glass of red wine. Maybe even white wine but I never asked.
Lessons Learned
Five-and-a-half weeks and have I learnt anything new that I would like to add to my Top Tips For Back Surgery from the first Journal?
1. Spinal surgery may often be better undertaken by an orthopaedic surgeon rather than a neuro-surgeon, however emotionally we are drawn to the neurologist when someone is operating around our spine.
2. The scale of the surgery should not always be the guiding factor. Sometimes big problems need big surgery, especially when the site is inherently inaccessible like the top of the lumbar spine. Focusing or opting for the ‘minimally invasive’ option will sometimes not necessarily get the job done.
3. Don’t always focus on the very unlikely and highly emotive complications – death, paralysis etc. I didn’t give them a moment’s thought. Much more useful is to focus on the more common (but still unlikely) side-effects – infection, weakness, non-fusion, ongoing pain, surgical bleeding requiring transfusion etc. I had a chronic lung infection after my 2013 surgery. I never expected a lung infection, but then again I never asked. I bloody well did this time.
4. Ask how many times the surgeon has performed your actual procedure and what is their success rate?
5. And the biggest of all. Know what the surgical plan is. Agree to the plan and also ask under what circumstances the surgeon will change the plan. In Mr Tucker’s case his opinion was that there would be no reason to change the plan. And he didn’t.
6. Despite the resistance is it not time we had a Trip Adviser type of website for surgeons? Why are they resisting it?
The good ones would come out well and the poor ones wouldn't. What's wrong with that?
Thank you
Lastly, thank you to Guy Andrews (@thecoureur / www.bluetrainpublising) for riding out to see me and also thank you to my client David, who as well dropping a 'get well' card into my house, spotted myself and Guy at Velo Life and secretly paid for our coffee and sandwich! What a lovely thing to do!